By Susan Greene, Colorado News Collaborative.
This investigation is part of the ongoing “On Edge” series about Colorado’s mental health by the Colorado News Collaborative, the nonprofit that unites more than 160 communities and news outlets like ours to ensure quality news for all Coloradans.
Matt Vinnola lay curled up on a downtown sidewalk one Sunday in September, his eyes as blank as those of the stuffed lamb he was using as a pillow. The former honors student and youth Taekwondo champion seemed too out of it to shoo a fly off his lip or realize he was peeing through his shorts onto the concrete. If he noticed the woman offering Wet Wipes or the man trying to hand him a $5 bill, he showed no interest.
“Tell them, just tell them I don’t need help, so stop it,” he grumbled to no one in plain sight.
The voices in Vinnola’s head whisper and yell. They can be so loud, so constant, he figures everyone can hear them. Chronic paranoid schizophrenia, and an addiction to shooting up whatever he can find to still the voices, have landed the 29-year-old Denverite in emergency rooms, psychiatric wards, and jails so many times that his mother stopped counting.
Crisis after crisis, Janet van der Laak had to push the Mental Health Center of Denver to provide care for her son instead of finding reasons to deny it. Each time the center dropped him from treatment, Vinnola lost more faith in seeking help. And the more faith he lost, the harder his mother pressed — because he was free falling and she alone could not catch him.

“What kind of safety-net system blows off the hardest cases?” van der Laak once wrote in a note to herself. “Giving up on Matt, giving up on anyone in crisis, should not be an option.”
As part of our ongoing “On Edge” coverage of mental health statewide, the Colorado News Collaborative has spent six months investigating a state behavioral health system that turns away some of the most vulnerable and at-risk Coloradans in crisis, with no recourse from state officials. We zeroed in on the 17 community mental health centers that are paid more than $437 million a year in tax dollars to serve as the core of Colorado’s safety net.
We learned that Colorado, the state with the nation’s highest rate of adult mental illness and lowest access to care, has been giving those centers non-compete contracts and a privileged rate status for nearly 60 years, without meaningful oversight.
Our investigation shows that the centers – most now facing workforce shortages – collectively have treated fewer clients during the pandemic than before it, despite skyrocketing mental health needs. At the same time, more than half the centers have been sitting on liquid reserves of $10 million or more. Denver’s center, which gave its CEO a bonus of more than $300,000 last year, kept more than $40 million in liquid reserves while its clients faced record-long wait times for care.
COLab also found that, starting long before the pandemic:
- The state’s payment system inadvertently created a financial incentive for the centers to take on fewer ill people and charge higher costs, while also protecting them from competition.
- The centers have been charging taxpayers up to 17 times more than independent Medicaid providers for the same services, but with little transparency about the expenses those rates are based on.
- Several centers, including those in communities with sizable immigrant populations, have had no Spanish-speaking care providers.
- Some centers have been paid for programs they’ve not provided, with no pushback from the state agencies funding – and charged with regulating – them.
We learned that some of these and other questionable practices stem from a long record by the centers’ powerful trade association of pressuring the state to avoid reforms that would ensure greater transparency and accountability.
Even now, as Gov. Jared Polis’s administration is poised to launch a new cabinet-level department to carry out those reforms, we’ve found that state government, at the urging of the trade group, is backpedaling. Months before the new Behavioral Health Administration even launches in July, state officials already have ruled out key ways of regulating the centers more closely. They also have all but scrapped what was supposed to be a top safety-net priority for the new department: Stepping in when the centers fail clients like Vinnola and trying to catch them before they hit bottom.
Colorado’s “safety net”
The community mental health movement took root in the 1960s when President John Kennedy called to deinstitutionalize people with mental illnesses. Private nonprofits popped up around Colorado to offer the mental health services – and, eventually, addiction counseling – needed to keep people out of hospitals, and in their communities.
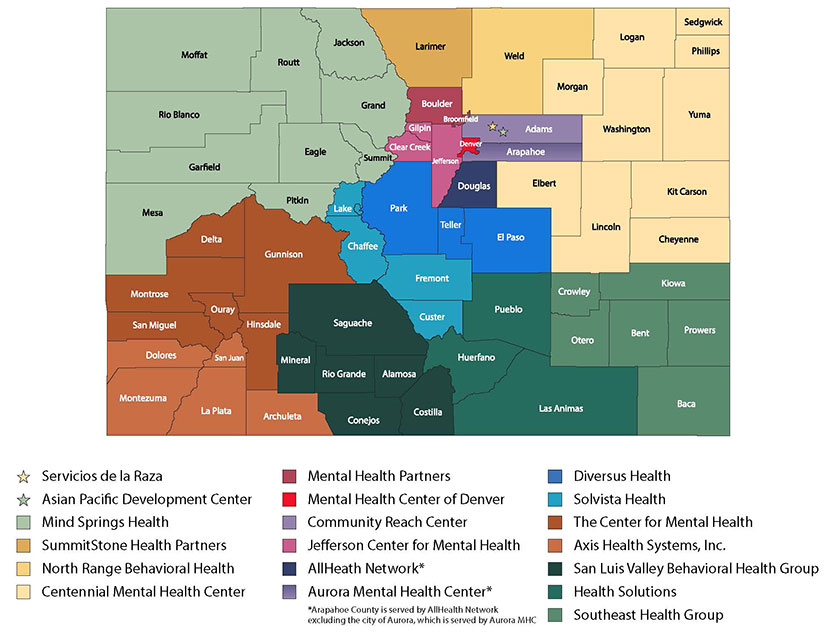
Those organizations eventually became the 17 regional community mental health centers (CMHCs) the state has relied on for more than a half-century to treat Coloradans who are indigent, on Medicaid or underinsured and can’t pay for private treatment, and to stabilize people in crisis. They are each contracted to provide inpatient hospitalization, intensive outpatient treatment, outpatient psychiatric care, counseling, and other forms of assistance to residents of the counties they’re responsible for serving.
The centers have helped generations of people throughout Colorado, especially those with less complex mental health needs. According to the state, they collectively served 158,911 clients in the fiscal year ending in June.
“Colorado is lucky to have the system it has built with such a strong network of CMHCs,” Doyle Forrestal, CEO of the centers’ trade group, the Colorado Behavioral Healthcare Council, wrote in an email.
Still, we found vast disparities in the quality and speed of the centers’ services.
Last summer, a Greeley resident with severe depression could see a psychiatrist within a few weeks of calling the center there, but someone just as depressed in Rio Blanco or Moffat counties had to wait 9 or 11 months, respectively, for the same kind of appointment, if Mind Springs Health – the center serving those counties – agreed to schedule one at all.
Multiple sources say at least four of the centers are providing addiction counseling by staffers who aren’t certified to counsel addicts. We spoke with people who either work in or with three centers that rely on clinicians with no pediatric training to prescribe medications to kids. Clients of four centers told us their clinics are so slow to renew prescriptions that they tailspin biochemically as they wait. And we found centers serving six communities with high immigrant populations that have no bilingual clinicians, leaving Spanish and other non-English speakers virtually iced out of care.
Annie Diaz of Cortez treated about 80 clients at a time as a counselor for Axis Health System – so many, she says she struggled to remember their names and problems. “I did the best that I could under the circumstances, but it wasn’t my best and it wasn’t good enough,” she says.
Some centers’ staffers describe pressure to drop their toughest cases. A former case manager at Mind Springs in Summit County says administrators made her stop treating an acutely ill client earlier this year because he made inappropriate racial comments. She says she objected because she knew he had no other support system, but complied for fear of losing her job.
The client ended his life shortly after.
“I blame myself for that every single day,” says the case manager, who quit right after his suicide. She asked to remain anonymous for fear the client’s death will hurt her career.
Mind Springs cited privacy reasons for refusing to discuss the case.
Emma Harmon, a single mom and Medicaid recipient in Durango, called Axis Health System when she was so depressed she was thinking about suicide several times an hour. She says the center made her wait six weeks for an intake appointment, then three more to meet with someone for a treatment plan. She asked to see a psychiatrist in the meantime, but was told he was busy. Her mother took her to the hospital, which released her because she hadn’t actually hurt herself.

Axis’ spokeswoman would not comment on Harmon’s case.
“I was on the brink of death – so, so close to killing myself, and they said ‘You’re fine’ and never followed up with me,” Harmon says. “The way things seem to work there, you’d actually have to have killed yourself before they’d meet with you…”

