The weird social virus known as Facebook has been with us for a number of years now, constantly mutating and defeating every attempt at control. It has reportedly infected 2.5 billion people worldwide. Other social media viruses — YouTube, Instagram, Twitter, WhatsApp — have infected somewhat lesser numbers of seemingly innocent people.
Some readers may remember the court case, last year, when Facebook agreed to pay a $5 billion penalty for illegally sharing user information. A Federal Trade Commission investigation had been set off by The New York Times and The Observer of London, which uncovered that the social network allowed Cambridge Analytica, a British consulting firm to the Trump campaign, to harvest personal information of its users. The British firm used the data to build political profiles about individuals — without the consent of Facebook users.
While we recognize that Facebook and other social media outlets serve as a way to ‘connect’ with friends and loved ones during enforced ‘social distancing’, we also realize that the algorithms used by social media outlets serve to amplify and spread ‘misinformation’ right alongside ‘valid information.’
Sheltering here at home, I find myself wondering how a relatively small number of public health experts — globally, a much smaller number than, say, the number of personnel in the world’s military forces — managed to shut down the economies and social institutions of every industrialized nation in the world, as ‘THE’ recommended way of combating an unfamiliar virus. International travel came essentially to a halt, as did domestic travel; entire industries closed their doors; classrooms were quite suddenly replaced by online Zoom chatrooms.
Could this have happened without Facebook and YouTube users sharing their concerns and fears with one another? (I ask this question, while noting that I used a couple of YouTube clips in this very editorial series.)
And could the shutdown of society have happened without a well-organized collaboration between public health workers and medical personnel?
According to BusinessWire.com (a Berkshire Hathaway company), the global healthcare market reached a value of nearly $8.5 trillion in 2018, having grown at a compound annual growth rate of 7.3% since 2014, and is expected to grow to nearly $12 trillion by 2022.
That’s ‘trillion’ with a ‘T’.
From BusinessWire.com:
Growth in the historic period resulted from the rapid growth in the elderly population, strong economic growth in emerging markets, decline in oil prices, and health insurance reforms globally.
Here are a couple of graphs, illustrating that growth within the US:

Up until about 1960, the healthcare industry as a whole consumed less than 5% of the nation’s Gross Domestic Product. By 2010, its portion of the GDP had nearly quadrupled. According to international research company IBISWorld, the healthcare industry now occupies the top two revenue-producing sectors in the US, generating a total of $2.2 trillion in revenues (not including the drug and cosmetics sectors):

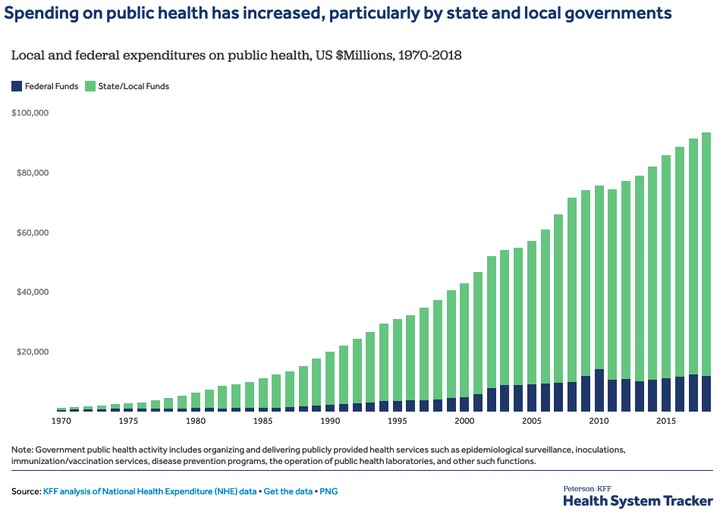
A very small part of the healthcare industry is occupied by the public health sector. Public health has been a well-recognized government function for at least two centuries, but here in the US, its importance seems to have grown exponentially since 1970, in terms of funding. As shown in the following graph, local, state and federal expenditures on public health increased from practically nothing in 1970 to more than $90 billion in 2018.
We’ve seen previous viral pandemics that killed thousands, or even millions, all around the world.
The Spanish flu (H1N1 virus) pandemic of 1918-1919, the deadliest in history, infected an estimated 500 million people worldwide — about one-third of the planet’s population at that time — and killed an estimated 20 million to 50 million victims, including some 675,000 Americans. The H1N1 flu was first observed in Europe, the United States and parts of Asia before swiftly spreading around the world. At the time, there were no effective drugs or vaccines were available, so citizens were ordered to wear masks… schools, theaters and businesses were shuttered… and bodies piled up in makeshift morgues before the virus ended its deadly global march.
Mortality was particularly high in people younger than 5 years old, in people 20-40 years old, and in people 65 years and older. The high mortality in healthy people, including those in the 20-40 year age group, was a unique feature of this pandemic.
While the H1N1 virus has been studied extensively by the CDC, the properties that made it so devastating are not well understood. With no vaccine to protect against influenza infection and no antibiotics to treat secondary bacterial infections that can be associated with influenza infections, control efforts worldwide were limited to non-pharmaceutical interventions such as isolation, quarantine, good personal hygiene, use of disinfectants, and limitations of public gatherings, which were applied unevenly.
To maintain morale in the midst of World War I, which was happening at the same time, government censors minimized reports of illness and mortality in Germany, the United Kingdom, France, and the United States. But newspapers were free to report the epidemic’s effects in Spain, because Spain was not involved in the war… and these stories created a false impression of Spain as especially hard hit, thus giving rise to the name ‘Spanish flu’.
Is COVID-19 so very different from the Spanish flu? Viewing the situation from the midst of the government-enforced lock-downs, we can feel like we’re going through something unique in the human experience, but in fact, research suggests that life during the Spanish flu was rather similar to what we’re now experiencing — except the death toll, then, was much higher.
We have new ways to communicate, however, in 2020. There was nothing similar to Facebook or YouTube in 1918. News traveled slowly, via telegraph or by mail, and was shared by popular newspapers and magazines. The ability to do a Google search, and confirm our favorite biases and prejudices, was absent.
And the healthcare industry was relatively minuscule in 1918 — consisting as it did mainly of independent family doctors who made house calls, and an occasional hospital operated typically by volunteers — nuns or other religious followers. The public health industry was even more minuscule — practically non-existent in most places.
The healthcare industry didn’t grow to mammoth size all on its own. Two important factors helped with that growth — the insurance industry, and the federal government’s Medicare and Medicaid programs. As shown in the chart above, the Health & Medical Insurance industry appears to be the second largest sector of the US economy, after hospitals. Larger than auto sales, larger than public schools, larger than commercial banking.
And we helped out as well. You and me and all of us. We demanded health insurance from our employers; we joined social media sites. We gave the healthcare industry the power to shut down the nation’s economy, and handed control of our communications over to Facebook.
We made our bed. Now we’re sleeping in it.

